Sickle cell patients in Kisumu County have petitioned the Social Health Authority (SHA) to classify the condition as a critical illness to cushion them against high costs of treatment.
Caroline Mabunde, a sickle cell warrior and advocate, said many patients were languishing at home without access to treatment amidst rising cases of the disease in Kisumu.
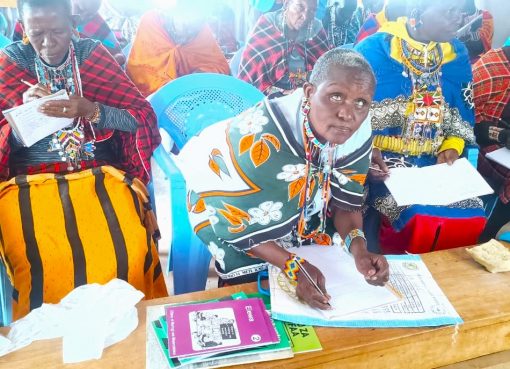
Speaking in Kisumu during a town hall meeting organised by Willow Health Media to take stock of SHA since it was rolled out in October last year, Mabunde said most of the health facilities in the area lacked essential drugs forcing patients to pay for treatment out of pocket.
Apheresis – a life-saving procedure used to reduce sickling crises, she said remains prohibitive to most of the patients since it is not covered under the current SHA benefit package.
“People are suffering in silence,” said Mabunde. “This is not just a treatment; for many of us, it is the difference between life and death. The costs are too high for ordinary families,” she said.
According to the latest data from Jaramogi Oginga Odinga Teaching and Referral Hospital (JOOTRH), Kisumu County has one of the highest cases of SCD in the country.
Approximately two out of every 100 children in Kisumu are born with sickle cell disease, and around 21 percent carry the sickle cell trait.
Most of the children do not live to celebrate their fifth birthday painting a grim picture of the management of the disease in the area.
Mabunde called for a review of the SHA benefits and packages to include SCD as a critical illness to ensure sicklers have access to the lifesaving procedure and treatment.
Under SHA, critical illnesses are primarily addressed through the Emergency, Chronic and Critical Illness Fund (ECCIF).
This fund is designed to provide financial protection for patients requiring intensive and specialized medical care, especially when costs exceed the limits of the standard Social Health Insurance Fund (SHIF).
Currently, apheresis, which is a specialized procedure often used in the management of sickle cell disease is not explicitly listed among the treatments covered under the ECCIF.
SHA Director of Provider and Beneficiary Management Hazel Koitaba said the concerns raised by the sicklers were valid.
Speaking during the same meeting, Koitaba said the Ministry of Health has prioritised the improvement of SHA through the recent appointment of a Benefits Package and Tariffs Advisory Panel.
She added that the panel, comprising experts in various fields like health economics and epidemiology was set to review benefit packages and tariffs under the SHA scheme assuring the sickle cell community that their plight shall be tabled before the team.
“We are aware of the challenges faced by sickle cell patients. Their plea is valid and will be given serious consideration during the benefit review process,” said Koitaba.
Other participants at the engagement forum echoed the need for increased support while commending the SHA for the progress it has made in expanding health coverage.
Kisumu County Director of Medical Services Dr Sunday Ogolla noted that over 580,000 Kisumu residents have been registered with the SHA and are receiving services from 255 public health facilities.
He added that SHA reimbursements have significantly boosted service delivery across the county.
Inuka Hospital Chief Executive Officer (CEO) Michael Adwera lauded and called for timely reimbursements to enable private health facilities to fill the gap in healthcare in the county.
Whereas the payments were consistently being channelled to the facilities, gaps still existed in the release of funds for theatre and operations.
“We don’t have a challenge with outpatient reimbursements but when it comes to theatre where operations consume the bulk of money in private facilities there’s some delay in reimbursement,” he said.
By Chris Mahandara