The national government has stepped up efforts to improve the standard of care in public health facilities with the launch of the Kenya Quality Model for Health Plus (KQMH+) programme, a new framework aimed at embedding safety, dignity and consistency in primary health care services across the country.
State Department for Public Health and Professional Standards Principal Secretary (PS) Mary Muthoni said the initiative signals a shift from merely expanding access to ensuring that the care patients receive is reliable and effective.
Speaking during the launch of the programme at Angola Health Centre in Kisumu County, the PS said KQMH+ brings together the national and county governments, development partners and frontline health workers to strengthen services at the primary care level, where most Kenyans first seek treatment.
“Universal Health Coverage (UHC) is not just about having a facility nearby or registering for health insurance. It is about what happens when a mother arrives in labour at night, when a child with pneumonia needs oxygen, or when an accident victim requires urgent care. Access without quality only creates uncertainty for patients and families,” she said.
The PS said the programme was anchored on recent health sector reforms, including the Primary Health Care Act, the Digital Health Act, the Facility Improvement Financing Act and the Social Health Insurance Act, all enacted in 2023.
She noted that these laws have created a legal and financial framework to ring-fence resources for health and strengthen service delivery at the grassroots.
The PS further linked the rollout to the proposed Quality of Health Care and Patient Safety Bill, 2025, which is currently before Parliament.
She said the bill seeks to establish clear standards on patient safety and create formal channels for patients to lodge complaints and receive redress with dignity.
“We want to move away from situations where patients feel neglected and only turn to social media to air their grievances. There must be a structured, respectful system where patients are heard and their safety is protected,” she said.
Muthoni added that KQMH+ will initially be implemented in more than 3,000 primary health care facilities in selected counties, with multidisciplinary teams supporting health workers to improve infection prevention, maternal and child health services, data use and referral systems. Digital tools will also be used for self-assessment and continuous quality improvement.
The KQMH+ programme, she said, would be scaled up through primary care networks, linking community health promoters, dispensaries, health centres and referral facilities into a more coordinated system adding that quality care must become the norm, not the exception, for every Kenyan.
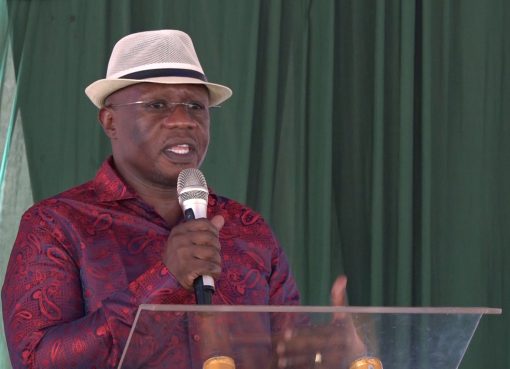
Kisumu Governor Prof. Peter Anyang’ Nyong’o, in a speech delivered by Deputy Governor Dr. Mathew Owili, said the county had already laid the groundwork for quality improvement through investments in infrastructure, staffing and digital systems.
He highlighted upgrades at several facilities, including Muhoroni County Hospital, where wards were refurbished and water and sanitation systems improved, and Lumumba County Hospital, which has been fully digitised using the TaifaCare system.
At Katito Sub-County Hospital, he said, the county has installed solar power, Wi-Fi and CCTV, transforming it into a 24-hour digitally enabled facility.
The governor said Kisumu has also strengthened maternity and emergency services, expanded specialist outreach in facilities such as Gita and Kombewa, and linked digital maternal health tools under the SafeMamaTech programme to the county’s Emergency Operations Centre and a 24-hour ambulance system.
He noted that the county executive had approved the recruitment of additional health workers to ease workload and improve responsiveness, particularly in maternity, outpatient and emergency departments.
Quality improvement, he said, has been integrated into routine operations, with dedicated allocations tied to facility funding.
PharmAccess, a key partner in the programme, said early results from quality improvement efforts in Kisumu were already encouraging.
Global Director for Quality Aafke de Graaff said compliance with infection prevention and control standards in supported facilities had risen from 60 per cent to 92 per cent.
She said stronger infection control practices including hand hygiene, proper use of protective equipment, safe waste management and improved ventilation were directly linked to better patient outcomes and lower risk of severe infections.
De Graaff noted that PharmAccess, through the SafeCare approach, supports health workers with practical tools that promote a culture of continuous learning and improvement rather than blame.
She added that digital technologies were increasingly enabling remote guidance, data-driven decision-making and stronger accountability across health systems.
By Chris Mahandara